If you or a loved one has been diagnosed with periosteal cloaking, you may find yourself with numerous questions. This rare radiographic phenomenon, commonly associated with specific bone conditions, often puzzles both patients and clinicians alike — especially among non-English speaking communities in places like Romania seeking reliable, localized health guidance.
In the United States, medical practitioners prioritize not just diagnostic accuracy but also ensuring that each patient fully comprehends their condition. Whether you’re navigating medical care through U.S.-affiliated telehealth networks, collaborating with local Romanian physicians interpreting international diagnostics, or exploring potential treatment plans across borders – understanding the nuances of **periostеal cloаking** is essential.
What is Periosteal Cloaking?
The phrase itself might conjure an almost poetic image – as if the protective sheath surrounding bone (known medically as the periosteum) is donning a metaphorical "cape" to hide its abnormalities. In medical imaging such as X-rays or CT scans, this visual distortion appears when abnormal soft-tissue inflammation overlays bony architecture in ways resembling a veil covering or altering the outline of cortical structures.
Why Does Periosteal Cloaking Happen? Exploring Common Causes
- Osteoid osteoma – frequently responsible for triggering subtle yet distinct radiologic findings including the so-called ‘cloaked’ effect around benign growths;
- Acute fractures or trauma-related healing stages,
- Certain types of
- Musculoskeletal infections like osteomyelitis, can generate sufficient tissue reaction and fluid accumulation near outer bone surfaces that alter traditional appearance patterns observed on routine imaging;
| Common Etiologies | Distinguishing Feature(s) |
|---|---|
| Traumatic Bone Injury | Recent history of physical impact; pain localization often matches injury location; |
| Bone Tumor (e.g., osteoblastoma) | Nighttime worsening discomfort relieved by salicylates suggests presence despite masking appearance; |
| Chronic inflammatory arthritis | Joint-centric pathology occasionally causes secondary periostal reactive patterns that mimic primary cloaking signs; |
| Rheumatological disorders (SLE/pseudotumoral form) | Multi-system symptoms alongside joint-bone interstitial involvement may create imaging illusions indistinguishable from direct osseous changes. |
Understanding the origin is pivotal to preventing misinterpretation; it's important that radiologists distinguish between true underlying lesions masked by surrounding tissue reactivity versus incidental overlapping soft tissue swelling.
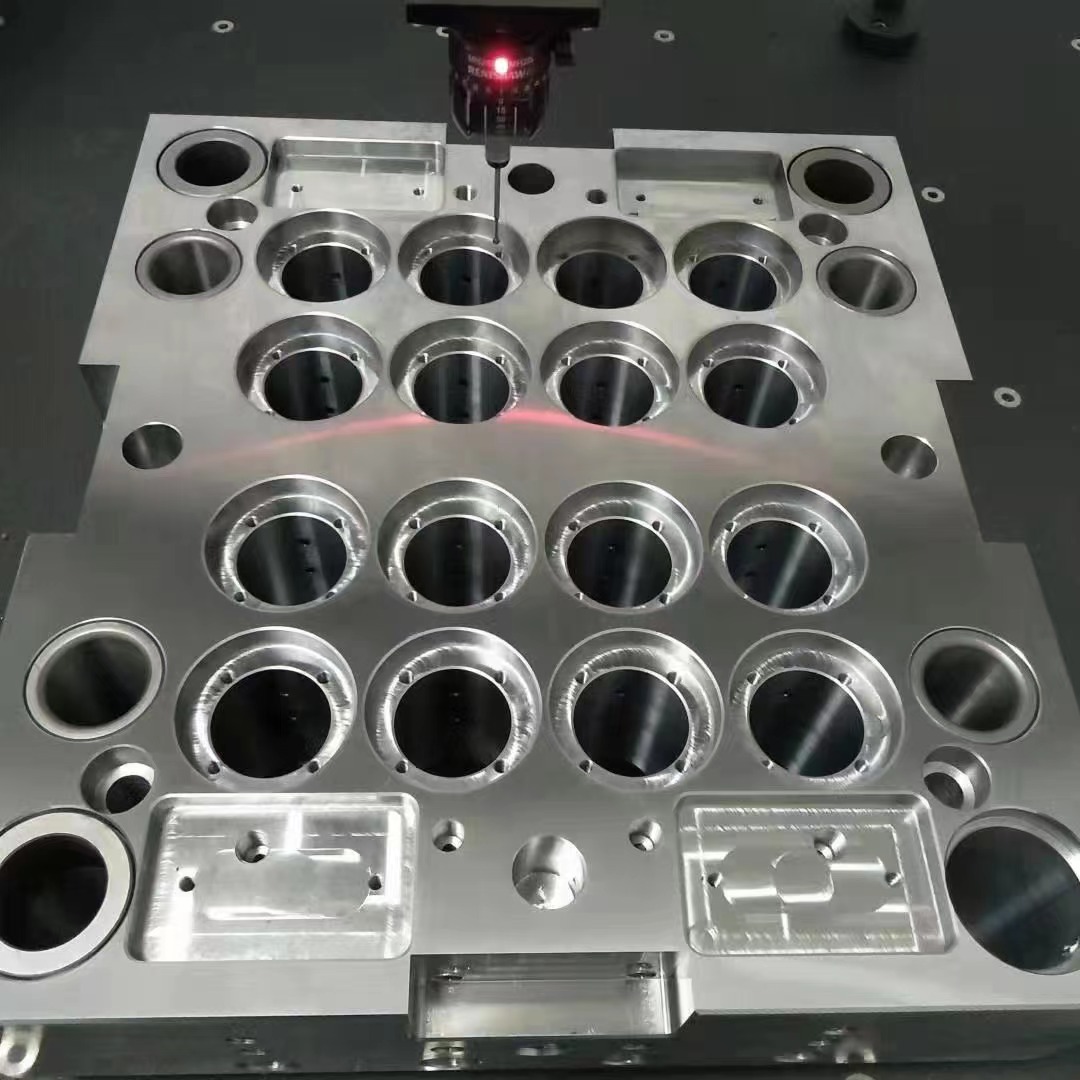
Key Diagnostic Methods Involved in Detection
The most widely accepted techniques employed for evaluating these findings include:
- Radiographs (X-Rays): Typically the first line of assessment. They help spot any deviation in bone structure although subtlety in this sign could be easily overlooked here;
- Magnetic resonance Imaging – superior capability identifying marrow edema, soft tissues alterations and pericranial reactions offering critical information not visible otherwise;
- Nuclear medicine scanning techniques: Particularly in diagnosing small nidus areas within suspected regions—such studies often guide more precise subsequent evaluations.
To summarize:
Clinical suspicion → Standard X-rays → Further cross-sectional imaging if findings equivocal or persistent clinical unease remains present
Identifying Typical Signs & Symptoms
“While the cloaking manifestation appears purely on imaging," explained leading orthopedic researcher Dr. Monica Langford MD/PhD in Boston’s Children’s Hospital Department during her grand rounds, “its root origins can have tangible impacts at the symptom level."Some manifestations include:
Patient complaints commonly reported are as follows:
- Local tenderness corresponding with site of perceived abnormal shadowing upon imagery
- Nights worsened dull ache, often alleviated temporarily using common pain medications (especially NSAIDs) suggesting metabolic-driven irritation likely tied to vascular-rich tumor activity beneath apparent 'mask’;
- Restricted motion due either to adjacent joint affection from proximity or reflexive muscle guarding;
However,
| Severity Grade | Pain Level Description | Likelihood of Soft-Tissue Reaction Seen in Visualizations |
|---|---|---|
|
|
Occasional, vague sensitivity; activity-independent | Faint trace, barely detectable (<20%) |
| II–Moderate | Rapidly escalating discomfort, especially nighttime exacerbations limiting restful sleep continuity | Localized thickening observed without dramatic structural loss indication(68%) |
| III | Continuous pain pattern persisting throughout daytime and intensified during weight-bearing movements(usually adolescents and active population subgroups) | Significant cloaking seen in all views - sometimes mistaken early-on for diffuse malignant infiltration until contrast enhanced MR clarifies true nature. |
An awareness of possible overlapping presentations ensures no red flags are missed while distinguishing mimics becomes crucial particularly amidst high anxiety scenarios (e.g post traumatic incidents following accidents.)
Current Treatment Approaches in U.S. Healthcare
Care plans vary considerably depending largely on what underlying process initially instigated this enigmatic pattern. Herein lies the reason why multidisciplinary teamwork is absolutely critical:
•Abscess-induced patterns: Prompt drainage coupled intravenous antibiotic protocols initiated once culture reports ready.
•In cases linked autoimmune dysregulation—immunosuppressive therapy adjustments along with biopsies being part of necessary diagnostic flowchart.